It’s an unsettling thought, but what if your eyesight suddenly started to slip away? Retinal detachment is an eye condition that can happen with little to no warning, often accompanied by symptoms like eye floaters. The good news? If caught early, it can often be treated successfully. DR LEE SHU YEN, Senior Consultant Ophthalmologist and Vitreoretinal Surgeon at Advanced Eye Clinic and Surgery, tells us all we need to know about retinal detachment so you know when to seek help.

What causes retinal detachment and how common is it?
The retina is the innermost layer of the eyeball. It contains nerve cells that transmit images to the brain to tell us what to see. A retinal detachment (RD) is the separation of the retina from the wall of the eye, usually secondary to a retinal break. This is a medical emergency, as the longer an RD is left untreated, the greater the risk of irreversible vision loss. RDs typically occur acutely, with a sudden onset of eye floaters and flashes, accompanied by a shadow in the field of vision that gradually increases in size. The main risk factors are:
#1 Age: In our 40s and 50s, the gel that fills the eyeball (known as the vitreous) undergoes liquefaction and collapses. Typically, this is a benign process and one only experiences transient flashes of light and some eye floaters. In some eyes, however, the vitreous may have abnormal adherence to the retina, and the collapse can cause the retina to tear, predisposing the eye to develop a retinal detachment.
#2 Myopia: Myopia, or short-sightedness, occurs when the eye is longer than normal. It requires glasses to refocus light rays onto the retina for sharp vision. In the myopic eye, the retina is stretched out and may have areas of thinning, known as lattice degeneration. These areas increase the risk of retinal tears and detachments. The higher the myopia, the greater the risk.
#3 Trauma – for example, a squash ball injury or a penetrating eye injury.
#4 Previous eye operations, such as cataract surgery. The prevalence of retinal detachments in Singapore is about 1 in 10,000, with Chinese men being at higher risk.
What are the symptoms of retinal detachment to look out for?
Retinal tears can cause detachments acutely, creating a medical emergency that requires surgical intervention to restore the eye’s anatomy and prevent vision loss.
In terms of symptoms of retinal detachment, typically the patient will report seeing hundreds of little black dots in the field of vision of one eye suddenly. These may be accompanied by flashes of light, which patients have described to be like lightning strikes at the side of their vision. If there’s no blurring of vision or shadow effect, there may only be a retinal tear without a retinal detachment. We can also use laser treatment to seal the edges of the tear and prevent progression to a retinal detachment. If a retinal detachment is present, the patient will notice a shadow in part of the field of vision. The shadow usually starts in the periphery and then progresses to affect the central vision as the area of retinal detachment increases.
To examine the retina, the ophthalmologist needs to dilate the pupil. They then use a device called a binocular indirect ophthalmoscope to examine the retina in detail. If a retinal detachment is present, they will see the affected area floating away from the inner wall of the eye. They can assess the extent of the detachment and document the location of any retinal tears.
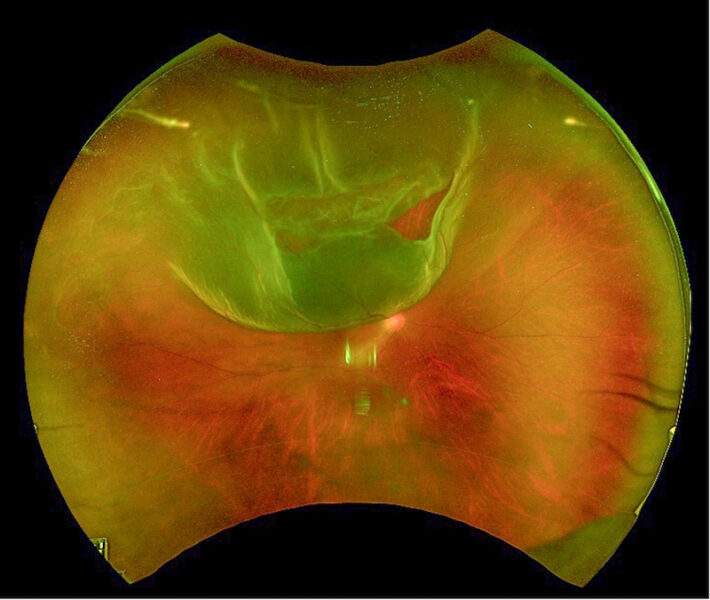
This image above depicts a retinal detachment in the right eye. We can see a retinal tear at the one o’clock position. The retinal detachment extends from the 10 to about two o’clock positions. This patient would have a sudden onset of eye floaters and about half the vision blocked by a shadow.
How can it be treated and managed?
Retinal detachments are medical emergencies that require intervention to restore the anatomy of the eye. The simplest method is a pneumoretinopexy, where a gas bubble is injected into the eye to close the incriminating retinal break and allow the fluid under the retina to be reabsorbed. This technique is only suitable for retinal breaks in the upper half of the retina. The patient has to maintain a head position to ensure closure of the break by the gas bubble.
The second type of surgery is a scleral buckle. This is akin to placing a belt around the widest part of the eye globe to provide an external indent that would close the retinal break.
The third technique, pars plana vitrectomy, involves removing the gel inside the eye (the vitreous), suctioning out the fluid under the retina and applying a laser around the retinal break. The surgeon then fills the eyeball with an inert surgical gas to hold the retina in place as it reattaches. Patients must maintain a face-down position to ensure the entire retina is protected by the gas bubble.
How serious can it get if left untreated?
Without intervention, a retinal detachment can progress and result in the complete separation of the retina, potentially leading to blindness. If the detachment has not yet affected the central retina (macula), surgeons should operate urgently to restore the eye’s anatomy and preserve good vision. However, once the macula is involved, it’s unlikely that vision will return to normal levels of 6/12 or better.
In general, more than 90 percent of acute retinal detachments can be successfully treated with a single operation. About 10 percent of cases may require repeat surgery due to scarring (proliferative vitreoretinopathy), new retinal breaks or failure of reattachment.
Advanced Eye Clinic and Surgery
3 Mount Elizabeth, #13-12
6517 9440 | advancedeyeclinic.sg | infolsy@aecs.sg
This article on eye floaters and symptoms of retinal detachment first appeared in the March 2025 edition of Expat Living. You can purchase the latest issue or subscribe so you never miss a copy!
Also, to make the most of living in Singapore, read our latest City Guide here for free!
Don't miss out on the latest events, news and
competitions by signing up to our newsletter!
By signing up, you'll receive our weekly newsletter and offers which you can update or unsubscribe to anytime.